The menstrual cycle is a fundamental aspect of reproductive health, serving as a barometer of overall well-being for individuals assigned female at birth. However, when menstruation is delayed without the presence of pregnancy, it can incite apprehension and uncertainty. In this in-depth guide, we embark on a journey to unravel the complexities surrounding maximum delay in periods if not pregnant. From physiological intricacies to lifestyle influences, we dissect the myriad factors that contribute to prolonged intervals between menstrual cycles, all while optimizing our understanding for search engines.
Understanding the Menstrual Cycle:
Delving into the intricacies of the menstrual cycle unveils a marvel of biological synchronization and hormonal orchestration. At its core, the menstrual cycle is a carefully choreographed series of events orchestrated by a delicate interplay of hormones. The journey begins with the menstrual phase, a period marked by the shedding of the endometrial lining that was built up in the previous cycle. Hormonal levels, including estrogen and progesterone, plummet, triggering the shedding of the uterine lining and the onset of menstruation. This phase, typically lasting 3-7 days, signifies both an end and a beginning, as the body prepares for a new cycle of fertility.
Following menstruation, the follicular phase emerges as the ovaries gear up for ovulation. Under the influence of follicle-stimulating hormone (FSH), ovarian follicles begin to mature, each housing an immature egg. As these follicles grow and develop, they secrete estrogen, initiating the process of thickening the endometrium in preparation for potential implantation. This phase, which typically spans the first half of the menstrual cycle, sets the stage for the pinnacle of fertility: ovulation.
Highlighting the typical duration of a menstrual cycle and variations within the normal range provides essential insights into the diversity of menstrual patterns among individuals. On average, a menstrual cycle spans approximately 28 days, although deviations from this duration are common and considered normal. However, it’s crucial to recognize that menstrual cycles can vary widely in length, with some individuals experiencing cycles as short as 21 days or as long as 35 days. These variations are influenced by numerous factors, including hormonal fluctuations, stress levels, lifestyle factors, and underlying health conditions. Understanding the spectrum of menstrual cycle lengths empowers individuals to recognize what constitutes normal for their bodies, fostering a deeper connection with their reproductive health and well-being.
Maximum Delay Without Pregnancy:
Exploring the concept of maximum delay without pregnancy sheds light on the range of normal variability in menstrual cycles and offers reassurance to individuals experiencing delayed menstruation. In the absence of pregnancy, it’s common for menstrual cycles to occasionally deviate from the typical duration. The maximum delay without pregnancy is typically considered to be between 21 to 35 days, although individual variations may occur. This means that a menstrual cycle may be considered normal even if menstruation occurs anywhere within this timeframe. However, it’s essential to note that persistent or significant deviations from one’s usual menstrual pattern warrant attention and may necessitate further investigation by a healthcare professional. By understanding the parameters of maximum delay without pregnancy, individuals can navigate their menstrual health with greater confidence and insight, knowing when to seek medical advice if necessary.
Stress and Its Impact:
Stress, a ubiquitous aspect of modern life, exerts a profound influence on various physiological processes, including the menstrual cycle. The intricate relationship between stress and the menstrual cycle underscores the interconnectedness of the mind and body. When confronted with stressors, whether physical, emotional, or environmental, the body’s stress response system, governed by the hypothalamic-pituitary-adrenal (HPA) axis, becomes activated. This triggers the release of stress hormones such as cortisol, which can disrupt the delicate balance of reproductive hormones involved in regulating the menstrual cycle.
Chronic or excessive stress can lead to dysregulation of the HPA axis, resulting in alterations to the menstrual cycle. For some individuals, stress may manifest as irregular or missed periods, while for others, it may exacerbate pre-existing menstrual disorders such as polycystic ovary syndrome (PCOS) or exacerbate symptoms of conditions like endometriosis. Additionally, stress can contribute to changes in menstrual flow, cycle length, and ovulatory function, potentially impacting fertility and reproductive health.
Moreover, stress-induced disruptions to the menstrual cycle can create a vicious cycle, whereby menstrual irregularities themselves become a source of stress, further exacerbating the problem. Recognizing the impact of stress on menstrual health is essential for fostering holistic well-being. Strategies to mitigate stress and promote resilience, such as mindfulness practices, relaxation techniques, regular exercise, adequate sleep, and seeking social support, can play a pivotal role in restoring hormonal balance and optimizing menstrual health. By addressing stress as a modifiable factor, individuals can cultivate a harmonious relationship between mind and body, fostering a sense of empowerment and balance in navigating the complexities of the menstrual cycle.
Hormonal Imbalances and Menstrual Irregularities:
Hormonal imbalances are often at the root of menstrual irregularities, disrupting the intricate hormonal orchestra necessary for a regular menstrual cycle. Conditions such as polycystic ovary syndrome (PCOS), thyroid disorders, and adrenal gland dysfunction can lead to fluctuations in estrogen, progesterone, and other reproductive hormones, impacting ovulation and menstruation. These imbalances may result in irregular cycles, anovulation, or amenorrhea. Additionally, hormonal contraceptives, while effective in preventing pregnancy, can introduce synthetic hormones that may alter menstrual patterns. Managing hormonal imbalances often involves a multifaceted approach, including lifestyle modifications, hormone therapy, and addressing underlying health conditions. By addressing hormonal imbalances, individuals can restore menstrual regularity and optimize reproductive health.
Nutritional Factors and Weight Changes:
Nutritional factors and weight changes exert significant influences on menstrual health. Inadequate nutrition can disrupt hormonal regulation, leading to irregular cycles or amenorrhea. Conversely, excessive weight gain or obesity can promote estrogen dominance and insulin resistance, contributing to menstrual irregularities. Moreover, extreme weight loss or being underweight can suppress ovulatory function, resulting in amenorrhea or oligomenorrhea. Balancing nutrition and maintaining a healthy weight are crucial for optimizing menstrual health and overall well-being. Seeking guidance from healthcare providers or registered dietitians can help address any nutritional deficiencies or excesses, promoting hormonal balance and regular menstrual cycles.
Medical Conditions and Their Influence:
Medical conditions can profoundly impact menstrual health, with various disorders affecting the intricate hormonal balance necessary for regular cycles. Conditions such as endometriosis, pelvic inflammatory disease (PID), and diabetes can disrupt ovulatory function and lead to irregular or painful periods. Additionally, chronic illnesses and their treatments may indirectly affect menstrual regularity. Managing these conditions through comprehensive medical care and targeted interventions is essential for optimizing menstrual health and overall well-being. Regular communication with healthcare providers can facilitate early detection and effective management strategies tailored to individual needs, promoting menstrual wellness and quality of life.
Medications and Menstrual Patterns:
Medications can significantly impact menstrual patterns, influencing the delicate hormonal balance that regulates the menstrual cycle. Certain medications, such as antidepressants, antipsychotics, and chemotherapy drugs, may interfere with the normal hormonal fluctuations necessary for regular menstruation. Additionally, hormonal contraceptives can introduce synthetic hormones that may cause changes in menstrual flow, cycle length, or spotting. Herbal supplements and over-the-counter medications may also affect menstrual regularity through their interactions with hormone levels or metabolic processes. Understanding the potential effects of medications on menstrual patterns is crucial for informed healthcare decision-making. Consulting healthcare providers can help navigate these complexities and mitigate any disruptions to menstrual health while managing medical conditions or addressing symptoms.
Environmental Exposures and Menstrual Health:
Environmental exposures have emerged as a growing concern in relation to menstrual health, as exposure to toxins, pollutants, and chemicals can disrupt hormonal balance and menstrual regularity. Endocrine-disrupting chemicals (EDCs) found in plastics, pesticides, and personal care products mimic or interfere with natural hormones, potentially leading to hormonal imbalances and menstrual irregularities. Additionally, exposure to environmental pollutants, such as air pollutants and heavy metals, has been linked to alterations in reproductive hormone levels and menstrual cycle disturbances. Minimizing exposure to these environmental hazards through lifestyle modifications and advocating for environmental regulations may help safeguard menstrual health and overall well-being.
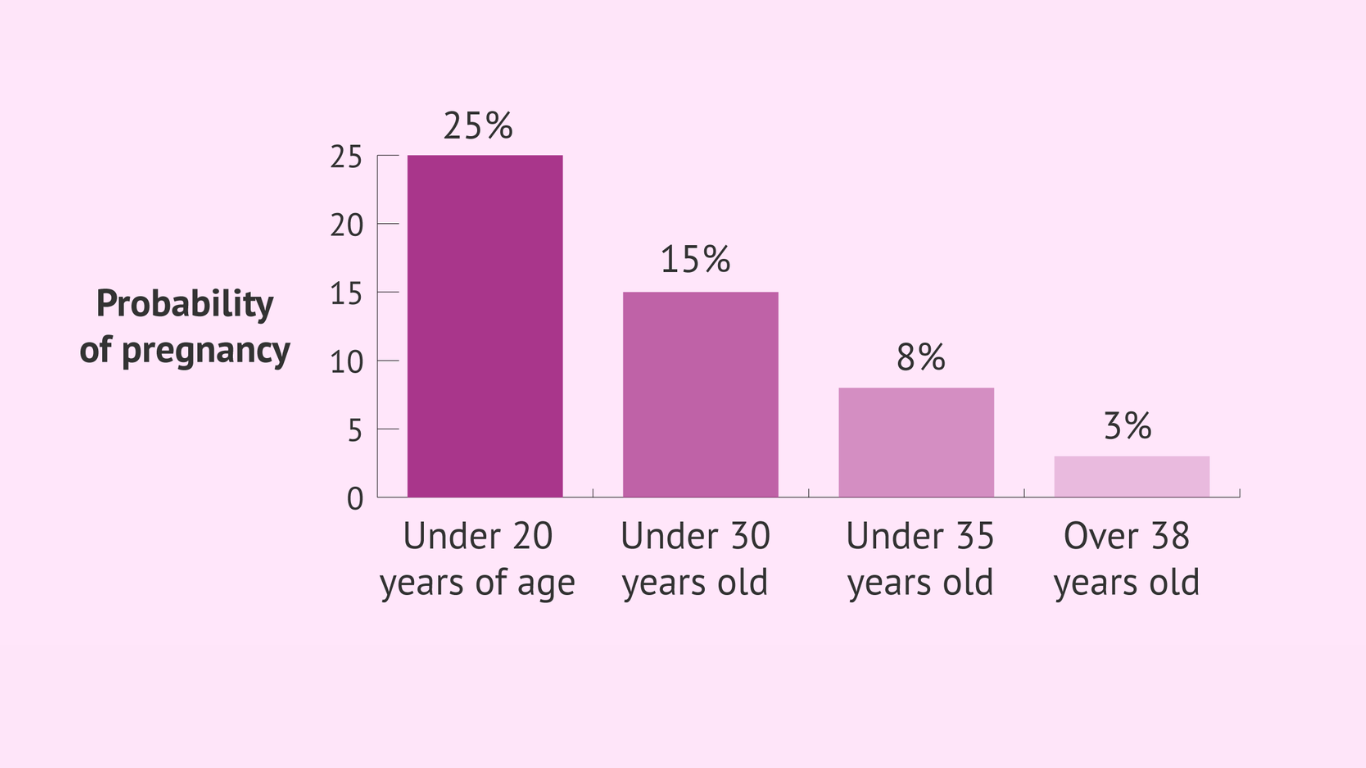
Age-Related Changes and Menstrual Patterns:
Age-related changes profoundly influence menstrual patterns as individuals transition through different life stages. Puberty marks the onset of menstrual cycles, typically characterized by irregularity and variability in cycle length as the reproductive system matures. As individuals approach menopause, hormonal fluctuations lead to changes in menstrual patterns, including irregular periods, shorter cycles, or skipped periods. Perimenopause, the transitional phase preceding menopause, is often accompanied by erratic menstrual cycles and symptoms such as hot flashes and mood changes. Understanding and adapting to these age-related changes are essential for maintaining reproductive health and well-being throughout the lifespan. Regular communication with healthcare providers can provide guidance and support during these transitions, ensuring optimal management of menstrual health.
When to Seek Medical Advice:
Knowing when to seek medical advice for menstrual irregularities is crucial for maintaining reproductive health and addressing underlying concerns. While occasional variations in menstrual patterns are common, persistent or significant changes warrant attention from healthcare providers. Red flags may include irregular cycles, unusually heavy or prolonged periods, severe menstrual cramps, or sudden changes in menstrual flow. Additionally, symptoms such as pelvic pain, abnormal vaginal bleeding between periods, or difficulty conceiving should prompt medical evaluation. Seeking timely medical advice allows for proper diagnosis and management of underlying conditions, ensuring optimal menstrual health and overall well-being.
Diagnostic Approaches for Menstrual Delay:
Diagnostic approaches for menstrual delay involve a thorough evaluation to identify underlying causes and inform appropriate management strategies. Healthcare providers may utilize a combination of medical history review, physical examination, and diagnostic tests to elucidate the root cause of menstrual irregularities. Common diagnostic modalities include pregnancy tests, hormonal assays to assess reproductive hormone levels, ultrasound imaging to evaluate pelvic structures, and endometrial biopsies to sample the uterine lining. These diagnostic tools help healthcare providers pinpoint potential contributing factors such as hormonal imbalances, structural abnormalities, or underlying medical conditions. By employing a comprehensive diagnostic approach, healthcare providers can tailor treatment plans to address individual needs effectively, optimizing menstrual health and overall well-being.
Treatment Strategies for Menstrual Irregularities:
Treatment strategies for menstrual irregularities aim to address underlying factors and alleviate symptoms to restore hormonal balance and promote menstrual health. Depending on the underlying cause, treatment may involve a combination of lifestyle modifications, hormonal therapies, dietary changes, and surgical interventions. Lifestyle modifications such as stress management techniques, regular exercise, and balanced nutrition can help regulate hormonal fluctuations and improve menstrual regularity. Hormonal therapies, including oral contraceptives, hormone replacement therapy, or medications to induce ovulation, may be prescribed to regulate menstrual cycles and alleviate symptoms. In cases of structural abnormalities or severe menstrual disorders, surgical interventions such as endometrial ablation or hysterectomy may be recommended. Individualized treatment plans tailored to specific needs and preferences can effectively address menstrual irregularities, enhancing overall well-being and quality of life. Regular follow-up with healthcare providers ensures ongoing monitoring and adjustments to treatment as needed, optimizing outcomes and promoting menstrual wellness.
In the intricate tapestry of menstrual delay, pregnancy serves as but one thread amidst a myriad of contributing factors. By delving into the multifaceted influences on menstrual regularity and embracing a holistic approach to reproductive health, individuals can navigate their menstrual journeys with confidence and empowerment. Armed with knowledge and proactive healthcare management, we can unravel the complexities of menstrual delay and pave the way toward optimal menstrual wellness, all while optimizing our content for search engine visibility.