In recent years, there has been a noticeable trend towards delayed childbirth, with many individuals choosing to start their families later in life. While this decision comes with its own set of joys and challenges, it’s essential to understand the unique aspects of pregnancy after the age of 35, often referred to as geriatric pregnancy. In this comprehensive guide, we’ll explore the facts, considerations, and expert advice surrounding geriatric pregnancy.
The Biological Clock and Fertility:
Understanding the Biological Clock:
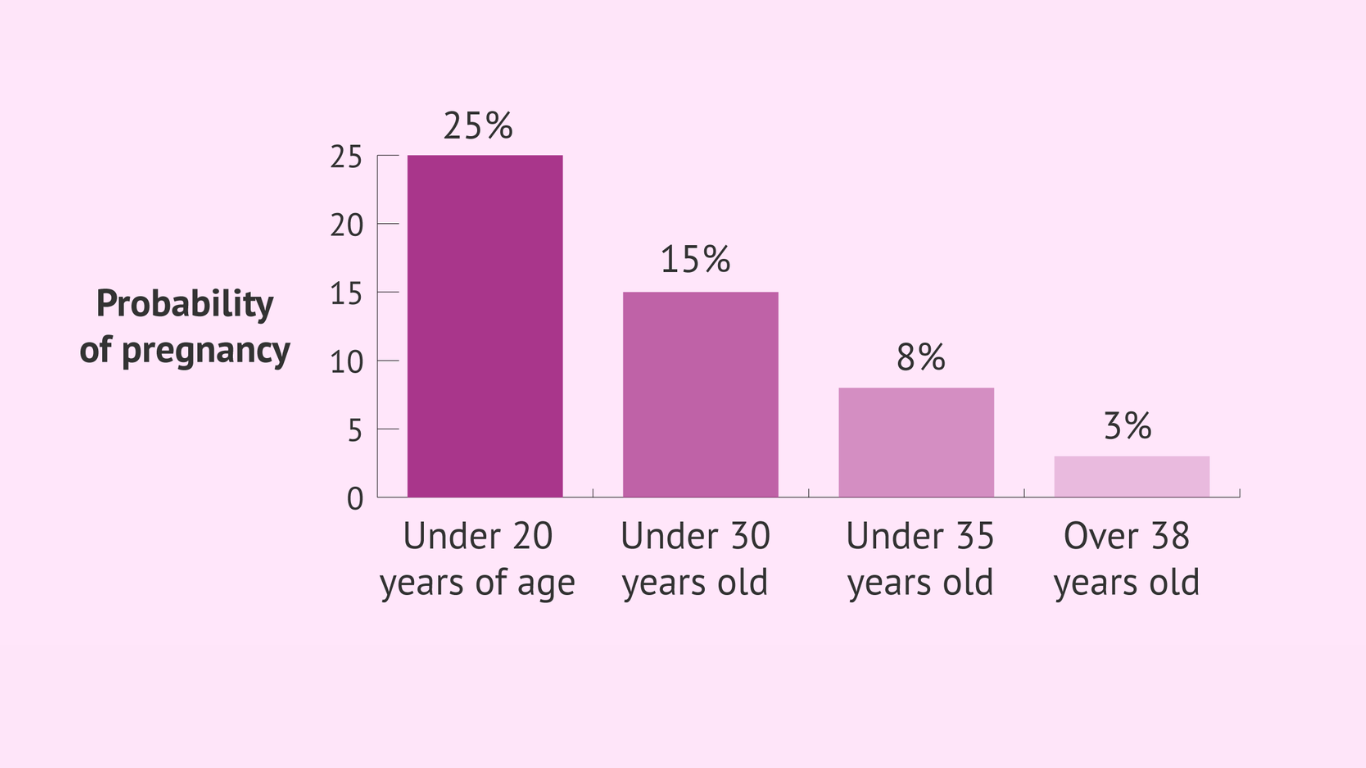
As individuals consider starting a family, the concept of the biological clock becomes increasingly relevant, particularly for women. The biological clock refers to the natural decline in fertility that occurs as women age, with a notable shift occurring after the age of 35.
Egg quality and quantity:
After age 35, women experience a decline in both the quality and quantity of their eggs. The genetic material within the eggs may be more prone to abnormalities, increasing the risk of chromosomal issues during conception. Additionally, the number of eggs available for fertilization decreases, making conception more challenging.
Fertility Challenges After 35:
Diminished Ovarian Reserve:
The ovaries house a woman’s eggs, and as she ages, the ovarian reserve, or the number of viable eggs, diminishes. This decrease in ovarian reserve can affect fertility and make it more difficult to conceive.
Assisted Reproductive Technologies (ART):
For those facing challenges in conceiving naturally, advancements in assisted reproductive technologies (ART) offer hope. Techniques such as in vitro fertilization (IVF) and egg freezing can help individuals preserve their fertility and increase the chances of successful conception.
Navigating Fertility Concerns:
Early Assessment and Planning:
Recognizing the impact of the biological clock, it’s advisable for individuals contemplating pregnancy after 35 to seek early assessment and planning. Fertility specialists can conduct tests to evaluate ovarian reserve and offer guidance on the most suitable paths forward.
Optimizing Conception Timing:
Understanding fertility patterns is crucial. Monitoring menstrual cycles, utilizing ovulation predictor kits, and engaging in regular sexual activity during fertile windows can enhance the chances of conception.
While the biological clock poses challenges to fertility after 35, proactive measures and advancements in reproductive technologies provide opportunities for individuals to navigate these challenges successfully. By understanding the impact of age on fertility and seeking timely assistance when needed, individuals can make informed decisions on their journey towards parenthood. The next sections of this guide will explore the increased risks and medical considerations associated with geriatric pregnancies, offering a comprehensive view for those embarking on this unique chapter of life.
Increased Risks and Medical Considerations:
As individuals choose to start their families later in life, commonly after the age of 35, it’s essential to be aware of the increased risks and medical considerations associated with geriatric pregnancy. This section delves into the potential challenges that may arise for both the expectant mother and the developing fetus.
1. Gestational Diabetes:
- Risk Increase: Women over 35 face a higher risk of developing gestational diabetes during pregnancy.
- Monitoring and Management: Regular glucose screenings and lifestyle modifications can help manage and mitigate the effects of gestational diabetes.
2. Preeclampsia:
- Higher Incidence: The risk of preeclampsia, a condition characterized by high blood pressure, increases with maternal age.
- Monitoring Blood Pressure: Regular blood pressure monitoring and prenatal care are crucial for early detection and management of preeclampsia.
3. Chromosomal Abnormalities:
- Increased Likelihood: Advanced maternal age is associated with a higher risk of chromosomal abnormalities such as Down syndrome.
- Screening and Diagnostic Tests: Prenatal screening tests, such as non-invasive prenatal testing (NIPT) and amniocentesis, can provide information about chromosomal health.
4. Cesarean Section (C-Section):
- Higher Probability: Geriatric pregnancies may have an increased likelihood of ending in a cesarean section, often due to factors such as fetal distress or complications during labor.
- Birth Plan Considerations: Expectant parents should discuss and be prepared for various birth scenarios, including the possibility of a C-section.
5. Preterm Birth and Low Birth Weight:
- Elevated Risks: Advanced maternal age is associated with an increased risk of preterm birth and delivering a baby with low birth weight.
- Prenatal Care and Monitoring: Regular prenatal check-ups, nutritional guidance, and monitoring can help address these risks.
6. Multiple Pregnancies:
- Higher Chance of Twins or Multiples: Older mothers, especially those undergoing fertility treatments, may have a higher chance of conceiving twins or multiples.
- Specialized Care: Multiple pregnancies require specialized medical care to ensure the well-being of both the mother and each baby.
While geriatric pregnancies come with heightened risks, it’s crucial to emphasize that many women over 35 have healthy pregnancies and deliver healthy babies. Regular prenatal care, open communication with healthcare providers, and lifestyle adjustments can significantly contribute to a positive pregnancy experience. The next section of this guide will explore the emotional and social aspects of delaying childbirth, providing insights into the unique dynamics individuals may encounter during this journey.
Emotional and social aspects:
Embarking on the journey of parenthood after the age of 35 introduces unique emotional and social dynamics. From societal expectations to personal reflections, this section explores the psychological aspects of delayed childbirth and offers insights into the emotional journey individuals may experience.
1. Societal Pressures and Expectations:
- Age-Related Stigma: Society may impose unwarranted stigmas on individuals choosing to start families later, leading to feelings of judgment and self-doubt.
- Empowerment Through Education: Understanding that delayed childbirth is increasingly common and backed by informed decisions can empower individuals to navigate societal pressures confidently.
2. Personal Reflections and Decision-Making:
- Balancing Career and Family: Many individuals delay parenthood to establish their careers. This decision often involves thoughtful consideration of priorities and the pursuit of a work-life balance.
- Self-Reflection: Engaging in introspective reflections about personal goals, values, and aspirations helps individuals align their decisions with their life path.
3. Psychological Impact of Advanced Maternal Age:
- Anxiety and Concerns: Older parents may experience heightened anxiety about their ability to keep up with the physical demands of parenting and ensure a healthy upbringing.
- Seeking Support: Open communication with healthcare providers and support groups can be instrumental in addressing concerns and providing reassurance.
4. Parenting Later in Life:
- Energy and Stamina: The physical demands of parenting may differ for older parents. Strategies for maintaining energy levels and overall well-being become crucial.
- Wisdom and Experience: Advanced age often brings a wealth of life experience, providing older parents with a unique perspective and valuable insights.
5. Support Systems and Social Networks:
- Building a Supportive Network: Establishing a strong support system is vital. This may include family, friends, and communities of individuals with similar experiences.
- Communicating Needs: Openly communicating needs and expectations with support networks fosters a positive environment for both the expectant parents and the baby.
Navigating the emotional and social aspects of delayed childbirth involves acknowledging and embracing one’s unique journey. By seeking support, maintaining open communication, and prioritizing self-reflection, individuals can approach geriatric pregnancy with confidence and resilience. The subsequent section will explore lifestyle and health optimization strategies, offering practical guidance on maintaining overall well-being during this significant life transition.
Lifestyle and Health Optimization:
Ensuring a healthy and thriving pregnancy after the age of 35 involves proactive lifestyle choices and focused health optimization. This section provides practical guidance on maintaining overall well-being and addressing the unique needs of individuals experiencing geriatric pregnancies.
1. Balanced Nutrition:
- Essential Nutrients: As the nutritional needs during pregnancy increase, focusing on a balanced diet rich in vitamins, minerals, and proteins is crucial.
- Supplementation: Consultation with healthcare providers can guide the appropriate use of prenatal vitamins and supplements.
2. Regular Exercise and Physical Activity:
- Customized Workouts: Tailored exercise routines that align with the individual’s health condition and stage of pregnancy contribute to overall fitness.
- Low-Impact Options: Engaging in low-impact activities, such as swimming or prenatal yoga, supports physical well-being without excessive strain.
3. Stress Management:
- Mindfulness Techniques: Incorporating mindfulness and relaxation techniques, such as meditation or deep breathing exercises, helps manage stress levels.
- Effective Time Management: Balancing work, personal life, and pregnancy requires thoughtful time management strategies.
4. Adequate Sleep:
- Quality Rest: Prioritizing sufficient and quality sleep is essential for the well-being of both the expectant mother and the developing baby.
- Comfortable Sleep Environment: Creating a comfortable sleep environment and adopting relaxation rituals contribute to better sleep quality.
5. Regular Prenatal Check-ups:
- Consistent Monitoring: Regular visits to healthcare providers ensure timely monitoring of the pregnancy’s progress and early detection of any potential issues.
- Open Communication: Establishing open communication with healthcare professionals allows for the discussion of concerns and the receipt of relevant guidance.
6. Avoidance of Harmful Substances:
- Tobacco and Alcohol: Eliminating or minimizing tobacco and alcohol consumption is crucial for the baby’s health.
- Caffeine Moderation: Limiting caffeine intake contributes to a healthier pregnancy.
7. Weight Management:
- Healthy Weight Gain: Achieving and maintaining a healthy weight throughout pregnancy is associated with positive outcomes for both the mother and the baby.
- Individualized Plans: Healthcare providers can offer personalized guidance on weight management based on individual health factors.
Lifestyle and health optimization play a pivotal role in promoting a positive geriatric pregnancy experience. By embracing balanced nutrition, regular exercise, effective stress management, and other proactive measures, expectant parents can enhance their well-being and contribute to the healthy development of their baby. The subsequent section will guide individuals on preparing for parenthood after 35, offering practical insights into creating a supportive environment for the growing family.
Preparing for Parenthood:
As individuals embark on the transformative journey of parenthood after the age of 35, thorough preparation and thoughtful considerations become essential. This section provides practical insights into creating a supportive environment, making lifestyle adjustments, and embracing the unique aspects of becoming a parent later in life.
1. Building a Supportive Network:
- Family and Friends: Establishing a reliable support system involving family and friends can provide emotional assistance and practical help.
- Parenting Communities: Joining parenting communities, both online and offline, connects individuals with others navigating similar experiences.
2. Healthcare and Prenatal Education:
- Choosing a Healthcare Provider: Selecting a healthcare provider experienced in geriatric pregnancies ensures comprehensive care.
- Prenatal Classes: Enrolling in prenatal classes offers valuable insights into childbirth, infant care, and parenting strategies.
3. Work-Life Balance:
- Communication with Employers: Openly communicating with employers about maternity leave, flexible work arrangements, and support policies contributes to a balanced work-life dynamic.
- Planning for Career Adjustments: Considering potential career adjustments to accommodate the demands of parenthood allows for a smoother transition.
4. Creating a Conducive Home Environment:
- Nursery Preparation: Setting up a comfortable and safe nursery space well in advance ensures a smooth transition for the baby.
- Home Safety Measures: Implementing safety measures, such as baby-proofing, contributes to a secure home environment.
5. Financial Planning:
- Budgeting for Parenthood: Evaluating and adjusting financial plans to accommodate the needs of a growing family is crucial.
- Insurance Coverage: Reviewing and updating insurance policies, including health and life insurance, ensures comprehensive coverage.
6. Embracing Parenting Wisdom:
- Grandparenting Insights: Leveraging the wisdom of older generations, such as grandparents, can provide valuable insights and support.
- Continuous Learning: Remaining open to continuous learning about parenting, child development, and evolving family dynamics contributes to effective parenting.
7. Self-Care and Couple Bonding:
- Prioritizing Self-Care: Allocating time for self-care activities, whether individually or as a couple, fosters overall well-being.
- Quality Time Together: Nurturing the couple’s relationship through quality time together contributes to a strong foundation for parenting.
Preparing for parenthood after 35 involves a combination of practical planning, emotional readiness, and a proactive approach to well-being. By building a robust support network, staying informed through prenatal education, and making necessary lifestyle adjustments, expectant parents can confidently navigate the challenges and joys of becoming parents later in life. As the journey unfolds, the support systems and preparations made during this period will contribute to a fulfilling and enriching parenting experience.
while geriatric pregnancy comes with its own set of challenges, being well-informed and proactive can significantly contribute to a healthy and positive pregnancy experience. By understanding the biological, medical, emotional, and lifestyle aspects, individuals embarking on the journey of parenthood after 35 can make informed decisions and ensure the best possible outcomes for both themselves and their newborns. Embracing the joys and addressing the challenges, geriatric pregnancy can indeed be a fulfilling and rewarding chapter in one’s life.